By Gerry Stanley, M.D. , May 5, 2022
There may be many ways to summit Mount Everest, but the safest route is to follow an established path with the help of a seasoned guide. The same advice holds true for exploring the latest and most promising innovation for treating patients suffering from chronic and acute pain: virtual reality.
Published Results for Vx(R) Therapy
The combination of virtual reality and behavioral health is a novel and effective option for resolving pain in the workplace, according to results of an article published on October 16, 2021, in the peer-reviewed journal “Pain and Therapy.” Study authors included myself, Chief Medical Officer, Harvard MedTech; A. Abd-Elsayed, Department of Anesthesiology, School of Medicine and Public Health, University of Wisconsin; and N. Hussain, Department of Pain Medicine, Beth Israel, Deaconess Medical Center, Harvard Medical Center.
The results reported in “Pain and Therapy” were achieved with a cohort of adult workers’ compensation patients aged 18 – 65 who were treated for acute or chronic workplace injuries from April 2019 to April 2020. All patients were referred to and overseen by a prescribing physician and referred to the Harvard MedTech Vx Pain Relief Program by orthopedic specialists, pain specialists, primary care physicians and occupational health providers.
Patients considerably reduced mean pain scores each week, averaging a reduction of 40% while using the virtual reality headset. In addition, their mean daily time spent thinking about pain symptoms decreased from 9.78 hours at the start of therapy to 2.76 hours after completing the 12-week program, representing a 72% reduction.
69% of Vx Patients Reported Decrease in Opioid Use
Reduction in reliance on opioids for pain control was also recorded, with 69% of patients reporting decreased opioid use. Patients experienced a 115% increase in their sleep duration and a 280% increase in the subjective quality of their sleep. Little attention is paid to sleep architecture and sleep hygiene in the workers’ compensation field. But when patients report that they are doubling the number of hours they are sleeping, it naturally translates into an environment where their depression, anxiety, PTSD and pain will improve, not to mention the underlying physical ailment driving their workplace injury.
As a result of these findings, we concluded that the Vx program – combining VR Therapy plus counseling – appears to provide meaningful reductions in pain and opioid use while improving the psychosocial aspects of trauma and pain, such as sleep, behavior, and physical activity.
Why Virtual Reality by Itself Isn’t Enough
Virtual reality has been explored for health care purposes for decades. Three factors are making it so impactful now:
Consider the mindset of a typical injured worker, someone who is depressed and isolated and removed from their familiar world. Imagine if you could allow that injured worker to disappear into a virtual world. They could leap down the rabbit hole for situational relief but not develop the skills necessary to achieve long-term healing. Combining that powerful escape mechanism with the guidance provided by a behavioral health specialist allows the patient to traverse their injury – both physical and psychological- without getting lost down the rabbit hole.
Moving Beyond Drugs and Surgery
Until now, the primary way to treat people with chronic pain or the effects of trauma was to use a biologically focused regimen of drugs, surgery, or a combination of both. Now we understand that targeted therapy using virtual reality and customized coaching can help the brain override the experience of pain, anxiety, and depression, without the potential dangers of drugs or surgery.
The impact of the virtual reality experience is supported by the Gate Control Theory of pain, which posits that alternative stimuli can reduce the intensity of physical pain by blocking pain messages at nerve gates in the spinal cord.
In essence, Vx Therapy has the ability to reprioritize the signals we are processing in our brains to promote long-term resiliency in patients.
Who Pays for This New Therapy?
As with any breakthrough solution, payment for these services is key to widespread adoption. Reimbursement for Vx Therapy is expanding among payers who recognize its value, especially when comparing it to the cost of prescription drug addiction, ongoing and even lifetime treatment, and/or additional surgeries that may not work. It’s especially gaining traction within workers’ compensation, where most injuries involve pain that, left untreated, can become long-term and expensive cases. It is important that a physician and or medical group partners with an experienced Vx provider who can work with them to ensure appropriate coding and reimbursement.
A New Model for Workplace Trauma
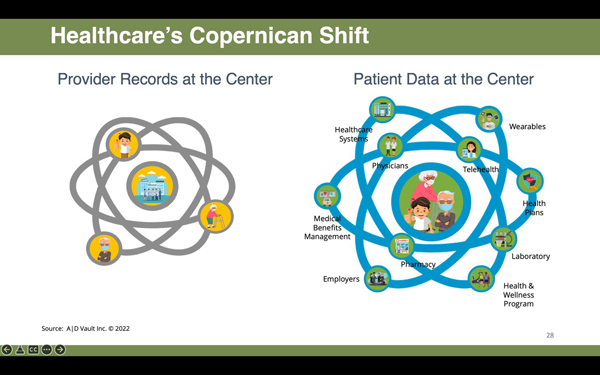
The combination of virtual reality and behavioral coaching within the Vx Therapy model activates the bio-psycho-social model for healthcare, first described by Dr. George Engle in 1977. So much of modern healthcare is focused on the biologic or physical aspects of disease. Now, the confluence of guided technology with behavioral coaching allows clinicians to engage and address the patient’s underlying psychologic and social factors.
The timing of this solution corresponds to the growing awareness of the role of behavioral health and recovery. The Orthopedic Forum recently published an article trying to understand and address the psychosocial determinants of health that derail orthopedic procedures. Many medical groups are trying to address this very topic. Vx Therapy has leaped to the forefront as a useful tool in addressing these silent aspects of patient care.
About the Author: Gerry Stanley, M.D., is Senior Vice President and Chief Medical Officer for Harvard MedTech. For more information, visit www.Harvardmedtech.com.

Leave A Comment